WHAT IS CAD?
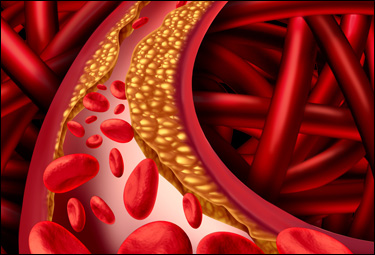
CAD - Coronary
Artery Disease - is a condition where fatty
pockets of material become lodged inside of
a wall of a coronary artery causing a
narrowing of that wall and decreasing blood
flow to the tissue serviced by that artery.
This narrowing is called
STENOSIS.
Your
body's natural healing process in such a
situation is to grow new artery wall over
the lodged material. This material
then becomes part of the artery. This
is bad because it is a foreign material and
it hardens over time - causing the artery
wall to become less flexible. Arteries
stretch during blood flow and their walls
are meant to be flexible.
This
lodged material causes a narrowing of the
artery which can lead to increased blood
pressure and stress on the artery itself.
Additionally it results in reduced blood
flow to the tissue serviced by the artery.
In time stenosis can worsen to the
point that blood flow becomes so restricted
that blood cells become lodged in the
narrowed opening resulting in a complete
blockage.
Other times for
reasons unknown the fatty pocket of material
under the artery wall ruptures out.
This activates your body's natural immune
response and platelet cells are sent to the
rupture and a clot is formed. This is
very bad for it takes an area already
restricted by stenosis and typically results
in a complete blockage.
In
both cases the end result is a heart attack.
|
 |
WHAT IS A
HEART ATTACK?
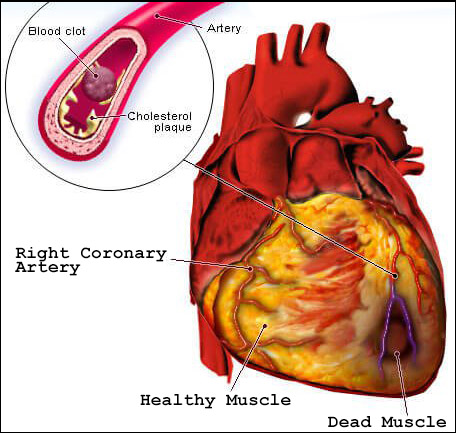
A
heart attack is caused whenever the blood
flow to cardiac muscle is reduced enough to
cause the heart's beating functions to be
reduced, affecting the delivery of oxygen
rich blood to the organs and tissues of your
body.
Also called a
myocardial infarction (MI). The reduction of blood supply to heart muscle
can rapidly damage and destroy heart tissue. This
is most often caused when plaque or a blood clot
reduces the space inside an artery lowering
the amount of blood able to pass through.
This reduces blood volume flow and causes
pain.
Unlike other types of muscle and tissue in your
body, heart tissue does not regenerate. When
it dies it remains dead. This means that if
enough heart tissue is destroyed during a heart
attack the heart can no longer function. This
is why heart attacks are often deadly and treatment
for a heart attack should be sought immediately.
A STEMI heart attack
is a complete blockage of a coronary artery
and if untreated STEMI heart attacks are
100% fatal.
|
 |
WHAT IS A WIDOWMAKER HEART ATTACK?
There are heart attacks and there are
STEMI heart attacks. A heart attack is
caused whenever the blood flow to cardiac
muscle is reduced enough to cause the
heart's beating functions to be reduced,
affecting the delivery of oxygen rich blood
to the organs and tissues of your body.
An ST Elevation Myocardial
Infarction (STEMI) heart attack
is a 100% blockage of a coronary artery.
The Widowmaker is a STEMI heart attack.
There are two main arteries that supply
blood to your heart, the Right Coronary
Artery and the Left Coronary Artery.
Arteries are like the branches of trees.
They split off into smaller branches several
times before reaching the cellular level
where oxygen is provided to your body's
cells. The main branch of the Left
Coronary Artery is the Left Anterior
Descending Coronary Artery or LAD for short.
The LAD is responsible for delivering 65% of
the oxygen rich blood needed to your heart
muscle. When the LAD blocks off,
tissue death occurs across a larger section
of your heart than if a smaller branch of
the LAD or of another coronary artery was
blocked.
Widowmakers are 100% fatal if not
treated. Even when treated they have a
90% mortality rate (9 out of 10 people die
from this type of heart attack).
In a
STEMI heart attack there is sudden rupture
of an unstable part of the wall in a heart
artery. This leads to a build up of clot in
an attempt to heal it however this clot
formation results in total blockage of the
artery. This total blockage leads to loss of
blood supply to the heart beyond that point.
The heart muscle stops working within
minutes and soon dies unless the blockage
can be cleared and the artery can be opened
back up. For this reason every minute from
the onset of a heart attack is absolutely
critical. Often the patient doesn�t make it
to hospital due to sudden death. For those
who put off seeking medical attention too
long or for those in whom the heart attack
isn�t treated a STEMI heart attack is 100%
fatal.
For those who do seek
medical attention and survive the initial
event the damaged or dead heart tissue
cannot be regenerated and they are left with
a damaged heart; healthy, normally
functioning heart tissue is replaced by a
non beating scar.

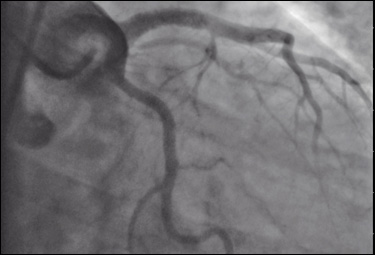
ABOVE: These are Summit4CAD Founder Jon
Patrick Hyde's Cardiac Cath Angiogram
images. In the left image (before
treatment) you can see that when compared to
the image on the right (after treatment)
that a blockage has occurred (no blood is
getting past the blockage and into the left
side arteries of the heart). The image
on the right shows Jon's heart after the
blockage has been removed and normal blood
flow has been established.
|
 |
WHAT IS
A CARDIAC CATH LAB?
The
full name is Cardiac Catherization
Laboratory - Cath Lab for short.
This is a specialized treatment facility
used to diagnose and treat coronary artery
disease. The procedures conducted in
the Cath Lab are an alternative to more
traditional open heart surgery.
Using x-ray machines which feed data to
the cardiologist real-time, the cardiologist
can diagnose and potentially treat CAD and
CAD related complications without putting
the patient through the stress of open heart
surgery.

|
 |
WHAT IS AN ANGIOGRAM?
An angiogram is a
non-emergency Cath Lab procedure used to
determine and diagnose CAD. A small
catheter is inserted through the femoral
artery in your leg and threaded up into the
heart. A dye that x-ray machines can
see is injected into your the arteries of
your heart so that the cardiologist can see
if there are any blockages or
stenosis
(narrowing of the arteries due to plaque
buildup).
|
 |
WHAT IS
AN ANGIOPLASTY?
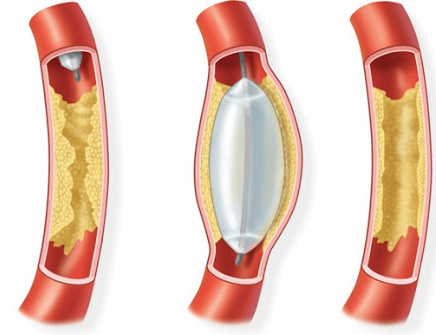
During
an angiogram the cardiologist may decide to
treat stenosis if any is present by
inserting a small balloon catheter into any
artery showing signs of stenosis. Once
placed in the area of narrowed artery the
cardiologist inflates the balloon and this
stretches the artery back open. This
is called a "Balloon Angioplasty".
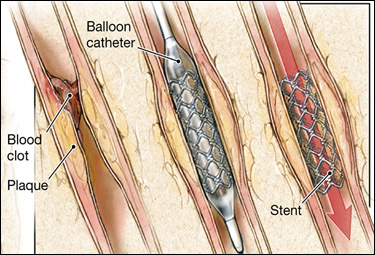
If the stenosis is significant the
cardiologist may be concerned that the
widening of the artery done with the balloon
catheter might not remain open and they may
decide to insert a "STENT".
|
 |
WHAT
IS A STENT?
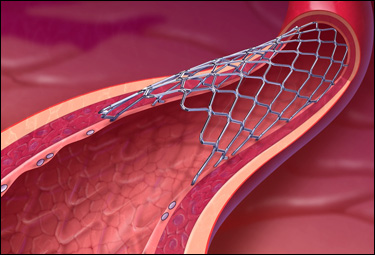
A stent is a
small piece of medication coated platinum
mesh that is inserted into a coronary artery
showing signs of significant stenosis
(narrowing). It is placed on a balloon
catheter. When the balloon is inflated
the stent stretches out and into the wall of
the artery holding it open. Eventually
the artery wall grows over the stent and it
becomes part of the artery structure.

 |
 |
WHAT
IS CCU?
CCU is the
Coronary Care Unit - it is sometimes
referred to as Cardiac Intensive Care Unit
or Cardiac Critical Care Unit. Think
ICU (Intensive Care Unit) but for heart
patients only. CCU is an intensive
care unit specifically designed and equipped
to care for critically injured or sick heart
(cardiac) patients.
Patients do not typically require CCU
stays after routine angiogram and/or
angioplasty procedures. If overnight
hospitalization is required patients are
typically sent to the PCU (Progressive Care
Unit).
CCU is reserved for
patients experiencing life-threating
conditions which require constant
monitoring.
|
 |
WHAT
IS CABG?
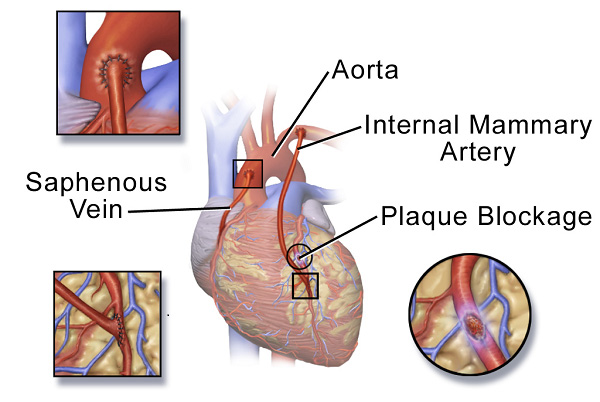
Pronounced
"Cabbage" - this is open heart bypass
surgery - called a Coronary Artery Bypass
Graft (CABG).
Before
angioplasty and stents this was the only
surgical treatment option for a blocked
coronary artery. The procedure is much
more dangerous and recovery takes much
longer. Additionally risk for
restenosis is high, meaning that additional
CABG procedures may be required in the
future.
A CABG procedure
consists of placing a graft between the IMA
(Internal Mammary Artery) and whatever
coronary artery is affected by the stenosis
or blockage. The graft is placed on
the side of the artery that is blocked -
bypassing the clot or stenosis so that blood
flow can resume to the affected tissue.
Up to 4 grafts can be attached to
the IMA - depending on how many coronary
arteries are affected - a patient can have a
single, double, triple or quadruple bypass
procedure.
 |
 |
|
WHAT ARE THE RISK FACTORS FOR CAD?
Risk factors for
CAD include:
-
Heredity - parents, grandparents,
uncles/aunts (blood related), siblings
- if any of these people have CAD or a
large number of risk factors for CAD you
may also be at risk.
-
High Blood Pressure - If
you have high blood pressure you are at
greater risk for CAD.
-
High Cholesterol/Borderline High
Cholesterol - high
cholesterol has been associated with the
building of plaque in coronary arteries
- which is the cause of CAD.
-
Diabetes -
Diabetes
causes high blood pressure and strain on
every organ system in your body.
-
Poor Diet - Foods high
in trans or saturated fats, high in salt
(sodium), or sugars, high in caffeine,
high in cholesterol - all contribute to
CAD.
-
Being Overweight or Obese
- Obesity puts additional
strain on your cardiovascular system and
heart.
-
Lack of Physical Activity
- Regular exercise is vital to a healthy
heart. Lack of regular exercise
can lead to worsening of risk factors
such as high cholesterol, diabetes, high
blood pressure and obesity.
-
Smoking - Smoking is
associated with several deadly diseases.
Smoking limits how much oxygen is
absorbed into your blood stream,
increases blood pressure, and can
increase cholesterol levels.
-
Stress - Research
shows that the most commonly reported
"trigger" for a heart attack is an
emotionally stressful event, especially
one involving anger. Stress
increases blood pressure.
-
Alcohol Consumption -
Heavy alcohol use can lead to high blood
pressure and can damage heart tissue.
-
Sleep Apnea - Sleep
apnea is a common disorder in which a
person has pauses in breathing while
they are sleeping or they breath
shallow, reducing the amount of oxygen
absorbed into the blood stream.
Untreated sleep apnea can lead to high
blood pressure, diabetes, stroke, and
heart attack.
|
 |
I
THINK I AM HAVING A HEART ATTACK, WHAT
SHOULD I DO?
Call 911 or
contact emergency services in the area where
you live immediately. Do
NOT drive yourself to the
hospital.
Most
importantly - REMAIN CALM! Many
heart attack victims suffer from elevated
stress or a panic attack as they are
experiencing their heart attack. It's
hard to not panic because frankly, it's
probably the most painful thing you'll ever
experience. It was for me. Even
if you are not in tremendous pain, it is a
very scary situation and it's
VITAL that you not give into
panic or fear. Focus on something that
keeps you calm and keeps you thinking.
**Panic causes your body to produce adrenaline
- which makes your heart beat faster.
If you are experiencing a heart attack,
making your heart beat faster may very well
cause your heart to fail completely.
I cannot stress
enough - stay calm and stay focused on
getting through your ordeal and being alive
and healthy when it is over. Doing
this will greatly improve your chances for
survival and recovery.
|
 |
|
WHAT ARE THE SYMPTOMS OF A HEART ATTACK?
It's important to
remember that symptoms of a heart attack
vary from person to person. Just
because you don't have shooting pain running
down your arm doesn't mean that the heavy,
crushing feeling you are experiencing in
your chest isn't a heart attack. My
pain was all the way across my chest - both
sides not just the left. And I had no
pain in my jaw or neck or back or arms.
I did have a tingling/numb sensation in my
fingertips and wrists. But the pain
was limited to my chest and never travelled
anywhere else. I certainly didn't have
the typical heart attack symptoms - but the
pain was beyond anything I'd ever felt.
So I knew it was something very serious.
If I had waited to get treatment I'd
probably not survived another couple of
hours.
Symptoms can be
different between men and women.
Likewise, women generally have higher pain
tolerances than men so their symptoms may be
much less severe.
Here is a list of
the most common symptoms experienced by
heart attack patients:
-
Chest Discomfort
- Pressure, squeezing, crushing
sensation, dull but intense pain.
This pain can be located towards the
left side of the chest, the center of
the chest, or across the entire chest.
Chest discomfort is the most common
symptom for both men and women.
This was the primary symptom
that I experienced.
-
Shortness of Breath
- with or without chest discomfort.
This is much more common in men that in
women.
I want to note that
I never experienced shortness of breath.
-
Pain in Other Areas of
The Upper Body - Pain in
your left arm or both arms, pain in your
jaw, back, or stomach. This is
less common in women.
I
want to note that I never experienced
any of these symptoms.
-
Diaphoresis (Cold
Sweats) - This is when you
feel cold but you are sweating
uncontrollably.
I DID
experience this symptom.
-
Nausea
-
Many heart attack victims mistake their
symptoms for food poisoning or the flu
because symptoms such as diaphoresis
when accompanied by nausea with stomach
pain and chest pain mask the true
underlying cause.
I never
experienced nausea or stomach distress.
-
Lightheadedness
- A large amount of blood is
pumped into your head each heartbeat to
keep oxygen flowing to your brain.
If your heart is compromised and not
pumping correctly a loss of blood volume
into your head will cause you to feel
lightheaded, dizzy, or even cause you to
black out.
I did not feel
lightheaded during my heart attack but
did experience it as a symptom a couple
of hours before my heart attack started
in full.
-
Numbness in Extremities
- Tingling fingers, numb hands or feet,
numbness in your wrists or arms.
It was this symptom that
actually convinced me that I was
experiencing a heart attack.
|
 |
I'VE
RECENTLY HAD A HEART ATTACK AND SURVIVED,
DOES THIS MEAN MY LIFE AS AN ACTIVE PERSON
IS OVER?
This is really
a difficult question. The truth is
that depending on the severity of your heart
attack and the amount of damage caused to
your heart tissue; you may be looking at a
greatly diminished quality of life.
CAD is the leading cause of early disability
retirement in adults in the United States.
The reason that
surviving a heart attack may mean a
significant change in your ability to be
active is simple : If
your heart has been damaged (meaning
there are areas of dead tissue that will not
regenerate) - your heart's ability to
pump blood is greatly affected
IN THE AREA that your heart
was damaged, but the rest of your heart will
continue to function as before.
THE DANGER IN THIS IS: that
if the damaged area(s) get out of sync with
the parts of your heart that are functioning
correctly (there are 4 chambers of your
heart that have to function together to
effectively pump blood) - your heart
could loose the ability to pump blood.
LIKEWISE -
there are "electrical nodes"
placed in different areas around your heart
that when activated cause your heart muscle
to contract (this is what keeps
everything working in order) -
think about the firing sequence of spark
plugs in your car's engine. If the
damaged/dead area of your heart contains one
of these very important nodes - your heart
can easily get out of sync because the "firing
order" of the electrical
impulses that cause your heart to function
correctly can get out of order. This
is called an "Arrhythmia"
and it is VERY DANGEROUS.
Arrhythmias can become deadly. They
are often caused when a damaged heart beats
faster (regular activities can cause this in
some post-heart attack patients if their
heart damage is significant).
I was facing this same possible
reality when I was sent home after my
hospital stay. I did exactly what my
doctor ordered (rest, relaxation, no stress,
no getting my heart worked up, no strenuous
activities, the AHA (American Heart
Association) diet, and take the medication
he prescribed to me which included a
medication that slowed my heart rate so it
could better heal.
I did these
things and when combined with the lifestyle
and fitness choices I'd made during the
course of my life I walked away from my
widowmaker heart attack experience with no
residual heart damage and a healthier, more
active lifestyle.
All of this
will depend on what your doctor(s) find when
they evaluate your heart post recovery.
This typically is done through a
diagnostic
test called an echocardiogram. This
test will give your doctor(s) the
information they need to determine what
activity level is safe for you. |
 |
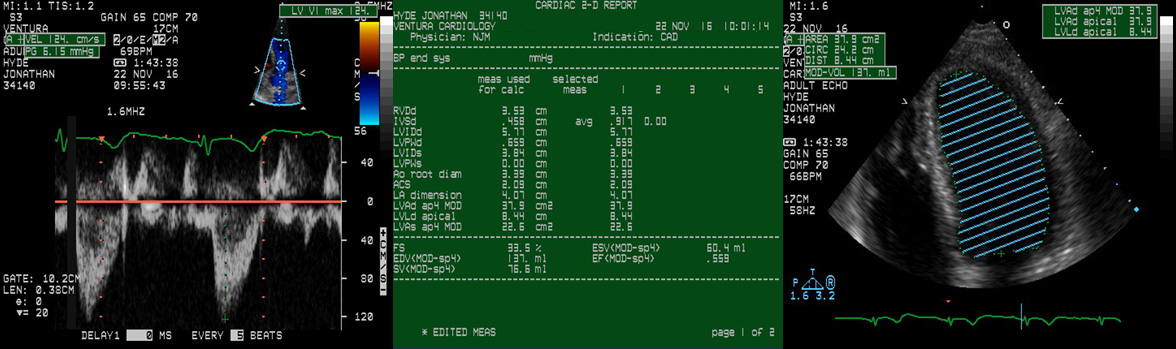
WHAT IS
AN ECHOCARDIOGRAM?
An
echocardiogram is a form of ultrasound
diagnostic test that is painless and usually
takes about 20 minutes to complete. It
offers an amazing array of diagnostic
information from how effective your heart's
chambers are in moving blood flow to how far
your heart muscle is contracting as it
beats. It provides an enormous amount
of data regarding the functions of your
heart.
|
 |
WHAT
ARE COLLATERAL ARTERIES?
Collateral Arteries are new artery
structures (which includes blood vessels and
smaller capillaries) that are grown as a
result of pushing your heart into a zone
beyond where it is getting adequate blood
supply during exercise. These new
"remodeled branches" - the medical term for
them - seem to be more common in people with
existing coronary artery disease.
These vessels provide an alternative source
of blood supply to the myocardium in cases
of coronary artery disease or an acute
(sudden) event such as a heart attack (where
blood flow to heart muscle is stopped).
Increasing evidence indicates that
collateral arteries provide a relevant
protective role in patients with coronary
artery disease.
Harvard Medical
School has released studies showing that
patients with CAD should focus on the
development of collateral arteries as a
means of reducing the negative health
effects of CAD and additionally minimize the
chance of permanent heart damage in patients
who experience a heart attack.
https://www.health.harvard.edu/press_releases/do-it-yourself-cardiac-bypass-surgery |
| |